Eligibility and Benefit Verification Services
Ensure Accuracy. Prevent Denials. Get Paid Faster.
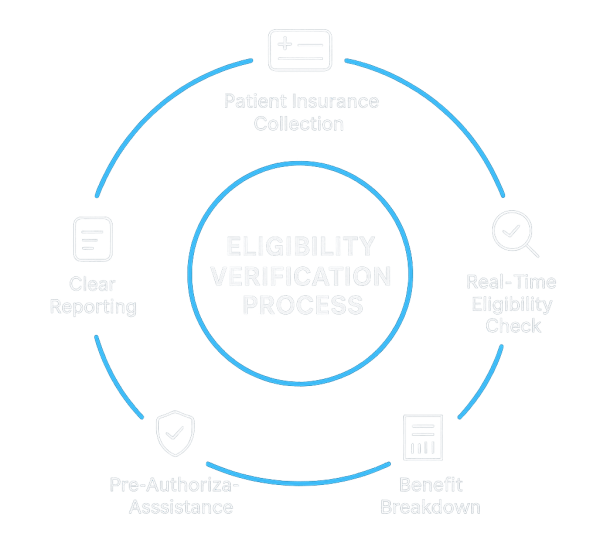
Managing insurance eligibility and benefits can be one of the most time-consuming tasks for healthcare providers. A single mistake can lead to claim denials, delayed payments, and frustrated patients. At MedRevenue Systems, we make this process simple and accurate, so you can focus more on patient care and less on paperwork.
Our verification services help you
Insurance Eligibility
Ensuring swift verification of patient insurance coverage with all payer types, maintaining up-to-date patient account records.
Benefits Verification
We ensure all patient details are up-to-date, covering benefits, deductibles, and policy status.
Referral Authorizations
We track and document the criteria for authorization or referrals to prevent revenue loss.
Accurate Documentation
Detailed and accurate documentation of all benefits, facilitating hassle-free billing.
Deductibles, Co-pays, and Co-insurance
Ensuring accurate calculations of patient deductibles, amounts met, and co-pays or co-insurance.
Efficient Workflow
Improve patient outcomes and boost revenue through our streamlined and efficient workflows.
Why Choose Med Revenue Systems
If you are in the medical, healthcare, dental, veterinary, or other field - we are here to help.
Accurate Verification
We carefully check every insurance detail to eliminate costly errors and ensure 100% accurate eligibility verification.
Real-Time Updates
Get instant and reliable information directly from insurance companies, helping you make quick and informed decisions.
Better Patient Experience
Patients are informed about their coverage, copays, and responsibilities upfront, reducing confusion in your Practice
Time Savings for Providers
Our team handles the complex verification process, giving your staff more time to focus on patient care instead of administrative work.
Revenue Protection
By minimizing denials and catching issues early, we help secure your revenue stream and prevent unnecessary financial losses.
No Long-Term Contracts
With our no- long-contract policy, you can cancel services anytime without any contract, setup, or training fees like other agencies have.
Call Now: 720-580-2331
Related Services
Virtual Medical Assistant
Enhance your practice with elite, highly skilled, and pre-trained virtual medical assistants.
Medical Billing Services
A cost-effective and adaptable billing solution with unmatched financial transparency.
Account Receivable
Track A/R trends, generate custom reports and monitor denials to boost collections and efficiency
Credentialing Services
Starting a new practice or adding a payer to your existing one? Partner with us to get started.
RCM Services
Discover how our comprehensive RCM services enhance efficiency and boost your revenue by increasing collections.
Eligibility & Benefits Verification FAQ’s
We verify details like coverage, copayments, deductibles, and coinsurance with the patient’s insurance provider. This process may also include checking for additional insurance coverage, the primary care provider (PCP), and the patient’s eligibility status.
We ensure billing alerts are provided at least 48 to 24 hours before the patient’s appointment and that demographic information is reported accurately.
To reduce denials, accounts receivable (AR) days, and revenue delays, verifying patient eligibility and benefits is essential. Confirming patient coverage before a visit facilitates timely collections. We identify and flag inactive plans, verify primary, secondary, and tertiary insurance, and check which services are covered under the patient’s policy. Additionally, we determine if a referral or prior authorization is required.
Most payers provide online interfaces for checking eligibility electronically before the scheduled patient appointment. However, it may occasionally be necessary to contact the payer directly to address questions about prior authorization requirements or to clarify specific aspects of eligibility and benefits.
What do our clients say?
MedRevenue Systems has been an incredible asset to our private practice, and I want to express my gratitude for their professional support over the past two years. I deeply appreciate their assistance with medical billing services, including eligibility and benefits verification, especially during the challenging time when our office manager, Jani, left. Since then, our partnership has been smooth and problem-free.
Get Started Today
Stop losing revenue to claim denials and slow insurance checks. Let MedRevenue Systems handle your eligibility and benefit verification with accuracy, speed, and compliance.

